FAQs: Acid reflux
- What is acid reflux?
- What is dyspepsia?
- I have a new irritating cough - could it be caused by acid reflux?
- What is GORD?
- What causes GORD?
- What's causing my acid reflux/GORD symptoms?
- Is there anything I can do for acid reflux/GORD/dyspepsia without taking medication?
- How can I treat acid reflux/GORD/heartburn/dyspepsia?
- What does PPI mean?
- How do PPIs work?
- Why are there so many different PPIs?
- Which PPI should I use?
- Do PPIs for acid reflux contain lactose/sucrose?
- What are the side effects of PPIs?
- Are there any long-term risks of taking PPIs?
- Can anyone take PPIs?
- I take other medicines - can I take PPIs?
- The PPI isn't working - what next?
- How soon should PPIs work?
- Does heartburn damage the heart?
- Is acid reflux/GORD/heartburn/dyspepsia dangerous?
- When should I consult a GP?
- Can antibiotics be used to treat acid reflux/GORD/heartburn/dyspepsia?
- Can I take a PPI in pregnancy or if I'm breastfeeding?
- I had an allergy reaction to Losec (or another PPI). Can I take a different PPI?
- I am due a medical investigation or blood test should I stop my PPI?
- Why can't I buy Zantac (ranitidine) anymore?
- What is H. pylori?
What is acid reflux?
As part of the digestive process, the stomach produces acid. This acid is meant to stay in the stomach but in some people it leaks into the bottom of the gullet (oesophagus) and it can then also travel up to the back of the throat. This causes a variety of symptoms including a burning feeling behind the breast bone (heartburn), sour/acid taste in the mouth and sometimes a persistent dry cough.
What is dyspepsia?
Dyspepsia literally means 'bad digestion'. In medical terms it encompasses a group of symptoms including upper abdominal discomfort, heartburn, acid reflux, nausea and/or vomiting, bloating, and burping. Most dyspepsia is termed 'functional' dyspepsia and is caused by a miscommunication between the gut and the brain, leading to oversensitivity of stomach nerves and overproduction of stomach acid.
I have a new irritating cough - could it be caused by acid reflux?
There are many causes for a cough, including acid irritation from reflux. A persistent new cough, especially if you are over 40 years old, should be checked by a GP and not assumed to be caused by acid reflux.
What is GORD?
GORD is Gastro-Oesophageal Reflux Disease. The US spelling is GERD - Gastro Esophageal Reflux Disease.
What causes GORD?
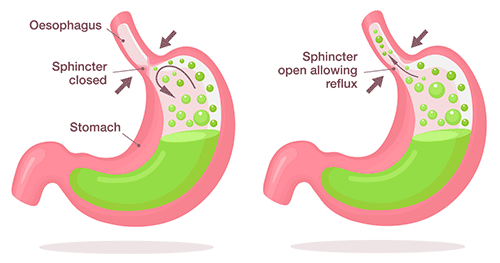
Gastro-Oesophageal Reflux Disease happens when stomach acid leaks into the gullet from the upper stomach, because the valve which keeps stomach contents in the stomach fails. The acid in the gullet causes irritation and inflammation. It can also reach the throat, causing irritation there and a cough.
What's causing my acid reflux/GORD symptoms?
Symptoms of acid reflux/GORD/indigestion are usually:
- A burning feeling in your chest behind the breastbone.
- An unpleasant acidic/sour taste in the back of your mouth.
Other symptoms can include:
- Nausea/vomiting.
- Bloating/belching.
- Chronic dry cough.
- Difficulty swallowing.
- Hoarse voice.
The symptoms should settle easily with occasional medication. Some of these symptoms can also be caused by more serious conditions, including cancers, so if you are unsure or they persist, discuss with a GP - do not self treat.
Is there anything I can do for acid reflux/GORD/dyspepsia without taking medication?
There are a variety of lifestyle changes which can help:
- Weight loss if overweight or obese - check using a BMI calculator.
- Avoid obvious trigger foods, e.g. cola, acidic fruits and acidic vegetables, fatty or spicy foods.
- Eat smaller portions and have your evening meal at least 4 hours before bedtime.
- Stop smoking - smoking increases the production of stomach acid.
- Reduce alcohol intake - alcohol (and cocaine) can cause inflammation of the stomach (gastritis).
- Look at ways to reduce stress and anxiety - these can trigger more acid production.
- Some other medications (especially anti-inflammatory tablets) can trigger reflux/indigestion - discuss with your GP if you think this may be the cause.
- Regular aerobic exercise (bending exercises not recommended with GORD).
How can I treat acid reflux/GORD/heartburn/dyspepsia?
As well as lifestyle measures, antacid medication in the form of tablets or chalky medicines which neutralise the stomach acid can help. More frequent problems can be helped by taking a PPI medication such as omeprazole (Losec), esomeprazole (Nexium), lansoprazole, or pantoprazole. These reduce production of stomach acid.
What does PPI mean?
PPI stands for Proton Pump Inhibitor.
How do PPIs work?
The 'proton pump' is the biochemical process which is used by the cells lining the stomach to make digestive acid in response to a meal. A Proton Pump Inhibitor blocks the pump so reducing acid production and reducing the level of acid in the stomach. As there is less acid, the symptoms of acid reflux and heartburn are reduced.
Why are there so many different PPIs?
The class of PPI medication was discovered in the 1970s, and omeprazole was the first one licensed in the UK. It was developed by AstraZeneca and sold as the brand 'Losec'. Other drug companies also developed their own PPI (e.g. esomeprazole and pantoprazole) by altering the chemical structures slightly.
Most PPIs in the UK are now out of patent and so generic versions are also available alongside the branded originals.
Research has shown that despite slight differences in the chemical structures all PPIs have very similar effects.
Acid reflux treatmentWhich PPI should I use?
Dr Fox offers a range of PPIs, as either capsules or tablets. They are all effective at treating symptoms of acid reflux/GORD/heartburn. It is best to take the lowest dose for the least amount of time.
- Losec/omeprazole 10mg capsules are the lowest dose to take once or twice a day.
- Nexium/esomeprazole and pantoprazole are stronger tablets (20mg) for once daily use.
- More people report side effects with lansoprazole and rabeprazole.
- Pantoprazole may be better for some people as there are fewer interactions with other medications and people report the fewest side effects with pantoprazole.
Comparing PPIs
| Brand name | Equivalent standard dose | Equivalent low dose | Tablets | Capsules | Orodispersible/melt in the mouth | Contains lactose | Number of common side effects reported | |
|---|---|---|---|---|---|---|---|---|
| Omeprazole | Losec | 20mg | 10mg | No | Yes | No | Yes | 8 |
| Esomeprazole | Nexium | 20mg | Not available | Yes | No | No | Some tablets | 8 |
| Lansoprazole | Zoton FasTab | 30mg | 15mg | No | Yes | Yes | Zoton FasTab | 15 |
| Pantoprazole | Not available | 40mg | 20mg | Yes | No | No | No | 1 |
| Rabeprazole | Pariet | 20mg | 10mg | Yes | No | No | No | 18 |
Do PPIs for acid reflux contain lactose/sucrose?
- Losec contains lactose.
- Generic omeprazole capsules often contain sucrose and some contain lactose.
- Nexium/esomeprazole tablets contain sucrose.
- Pantoprazole tablets do not contain sucrose or lactose.
- Zoton FasTabs contain lactose but generic lansoprazole capsules and orodispersible tablets do not contain lactose.
- Neither Pariet nor rabeprazole gastro resistant tablets contain lactose.
What are the side effects of PPIs?
Most PPIs have a similar range of possible side effects, though not everyone will get them. Pantoprazole users report fewer side effect problems.
Side effects can include:
- Headache.
- Constipation or diarrhoea.
- Flatulence (wind).
- Nausea/vomiting.
- Stomach pains.
- Small harmless stomach polyps (only seen on endoscopy and settle on stopping medication).
Are there any long-term risks of taking PPIs?
Taking PPIs daily for a long time has been linked with some other medical problems.
- Low magnesium levels - PPIs reduce absorption of magnesium in the intestine. If taken for longer than 3 months continuously, this can cause magnesium levels in the blood to drop. This can be worse if also taking other magnesium lowering tablets (e.g. Digoxin). Symptoms include fatigue, dizziness, confusion, fits, and irregular heart rhythms. Some GPs recommend regular magnesium blood checks, after 3 months use.
- Low vitamin B12 levels - the body needs stomach acid to absorb vitamin B12. If there are already reduced body stores of vitamin B12, or after long-term use, the levels may become too low. This can lead to anaemia. See a GP who can arrange a blood test if you have any symptoms or concerns.
- Bone fractures - there is a slight increase in the risk of fractures especially of the hip, wrist and spine. Patients are recommended to discuss long term use with a GP and to follow national guidelines for prevention and treatment of osteoporosis, including an adequate intake of calcium and vitamin D. Risk is further increased if also taking regular steroid medication.
- There is a slightly higher risk of catching diarrhoea and vomiting caused by Campylobacter or a Salmonella, as stomach acid plays a protective role against D&V/gastroenteritis bacteria.
- There is a very small risk of developing a very rare skin condition subacute cutaneous lupus erythematosus (SCLE). Consult your GP promptly, if you develop a skin rash on sunlight exposed areas.
- Research published in 2023 seems to show a link with long term use of PPIs and the development of dementia in later life. More research is needed to clarify this.
Can anyone take PPIs?
Short term PPI treatment is generally very safe.
However PPI treatment should be supervised by a GP/specialist in certain situations:
- Long-term continuous use.
- You may need extra blood test monitoring if taking phenytoin (for fits) or warfarin type anticoagulants (blood thinners requiring regular blood tests).
- PPIs interact with some other medicines and in particular may make some treatments less effective - these include HIV/AIDS treatments and some cancer chemotherapy, including high dose methotrexate.
- If there is severe liver or kidney disease, they may not be suitable.
I take other medicines - can I take PPIs?
PPIs do interact with some other medications. Checks are carried out in the online consultation and there is more information in the patient information leaflets included in the packet of individual medications. Anybody taking regular medication should let their GP know they are taking occasional PPIs. The GP may want to monitor the regular medication or adjust the dosages.
A wide range of medications can cause or worsen symptoms of dyspepsia and GORD. Check the patient information leaflets included in your medication and if in doubt consult your GP.
The PPI isn't working - what next?
If taking the medication at the recommended dose does not help your symptoms at all within 2 weeks, or symptoms recur immediately on stopping, or you find you need to take it every single day to control symptoms, consult a GP for further investigations.
How soon should PPIs work?
Most people with simple acid reflux/GORD/heartburn/dyspepsia/indigestion will find good relief of their symptoms within a few days. Symptoms should settle within 2 weeks. Consult a GP if you have ongoing problems.
Does heartburn damage the heart?
Heartburn has nothing to do with the heart. It is a symptom of acid in the gullet (oesophagus). It does not cause heart problems.
Is acid reflux/GORD/heartburn/dyspepsia dangerous?
Many people suffer from occasional acid reflux/GORD/heartburn which settles quickly and easily with occasional medication.
If symptoms are left untreated, then more severe damage could develop in the oesophagus leading in rare instances to ulcers, scarring, narrowing or permanent cell changes (Barrett's Oesophagus). There is a very small risk of these changes leading to cancer in the gullet.
Acid reflux/GORD/heartburn/dyspepsia/indigestion can also be signs of more serious health conditions, including cancers. If it doesn't settle easily or persists frequently, consult a GP.
When should I consult a GP?
As there is a risk of PPI treatment hiding more serious illness, it is important to be sure of a diagnosis of simple acid reflux/GORD/heartburn.
Consult a GP if:
- You are not sure about the symptoms or have never seen a doctor about acid problems.
- You are over 55 years with new symptoms in the last year or with symptoms that are worsening or changing.
- You have acid reflux/GORD/heartburn/dyspepsia with any of the following:
- Unintentional weight loss.
- Anaemia (pale and lethargic).
- Difficulty or pain on swallowing.
- Frequent vomiting, particularly if there is blood in the vomit.
- Black, shiny or bloody stools, or new persistent diarrhoea.
- Previous gastric ulcer or gastric surgery.
- Jaundice or severe liver problems.
- Persistent upper abdominal pain or new unexplained abdominal lump.
- You have had to take an antacid or acid suppressor continuously for four or more weeks in order to control symptoms.
- You have taken an indigestion or heartburn remedy for two weeks with no relief of symptoms.
- Symptoms return immediately on stopping tablets.
- You need to take a PPI on most days after completing the initial course.
Can antibiotics be used to treat acid reflux/GORD/heartburn/dyspepsia?
Sometimes acid reflux/GORD/heartburn/dyspepsia can be linked to long-term infection in the stomach with H. pylori. A GP may arrange a test for this. The test is usually either a simple breath test or stool (poo) test (home self tests are also available). For the test to be reliable, you must not have taken a PPI in the past 2 weeks, or antibiotics in the past 4 weeks. If the H. Pylori test is positive, a course of antibiotic treatment alongside a PPI is usually prescribed.
Can I take a PPI in pregnancy or if I'm breastfeeding?
You must discuss this with your GP/specialist as no medication should be taken in pregnancy or whilst breastfeeding unless absolutely necessary. Dr Fox does not supply for use whilst pregnant or breastfeeding.
Losec/omeprazole seems to be safe and may be taken in pregnancy and when breastfeeding if your GP or specialist advises to do so. See Best use of medicines in pregnancy - omeprazole.
There is no information available about safety in pregnancy or breastfeeding for Nexium/esomeprazole or pantoprazole and they should generally not be used. Pantoprazole is secreted in breast milk.
Further information: Use of Proton Pump Inhibitors (PPIs) in pregnancy.
I had an allergy reaction to Losec (or another PPI). Can I take a different PPI?
No. This often means that you will also react to the other PPIs.
If you have any symptoms or signs suggestive of an acute allergic reaction (anaphylaxis), you must get medical help immediately (telephone 999 if in the UK).
Symptoms/signs of an acute allergic reaction include:
- Difficulty breathing, tight chest, wheezing.
- Swelling of the face, lips, or tongue.
- Skin rash - urticaria/hives.
- Confusion/collapse/unconsciousness.
I am due a medical investigation or blood test should I stop my PPI?
Possibly. PPIs can interfere with the results of some blood tests, or hide serious conditions during endoscopy. Let the doctor or nurse know that you are taking a PPI. You may have to stop it for up to a few weeks, to prevent it interfering with the results.
Why can't I buy Zantac (ranitidine) anymore?
Zantac/ranitidine was withdrawn by the manufacturers in October 2019, due to the discovery of the contaminant N-nitrosodimethylamine (NDMA) which has genotoxic and carcinogenic potential - further details. It is unclear if and when production will start again (April 2024). Although Zantac is from a different class of drug (H2 receptor antagonists), the PPIs Losec (omeprazole), Nexium (esomeprazole), lansoprazole, or pantoprazole can be taken as an alternative.
What is H. pylori?
H. pylori stands for Helicobacter Pylori which are bacteria that can live in the stomach and cause inflammation. It is thought up to 40% of the UK population has this in their stomach but it does not cause any problems in 80-90% of these people. In those that it does cause symptoms, it can lead to stomach or duodenal ulcers. If symptoms of heartburn or reflux do not settle with treatment then it is recommended to have a test to check if H. pylori is present. This is usually done through a stool test although it can also be performed via a breath test.
Acid reflux treatment
Authored 11 March 2021 by Dr A. Wood
MB ChB Manchester University 1984. Former NHS GP in Bristol. GMC no. 2855422
Reviewed by Dr C. Pugh, Dr B. Babor
Last reviewed 21 December 2023
Last updated 12 March 2025
Editorial policy


